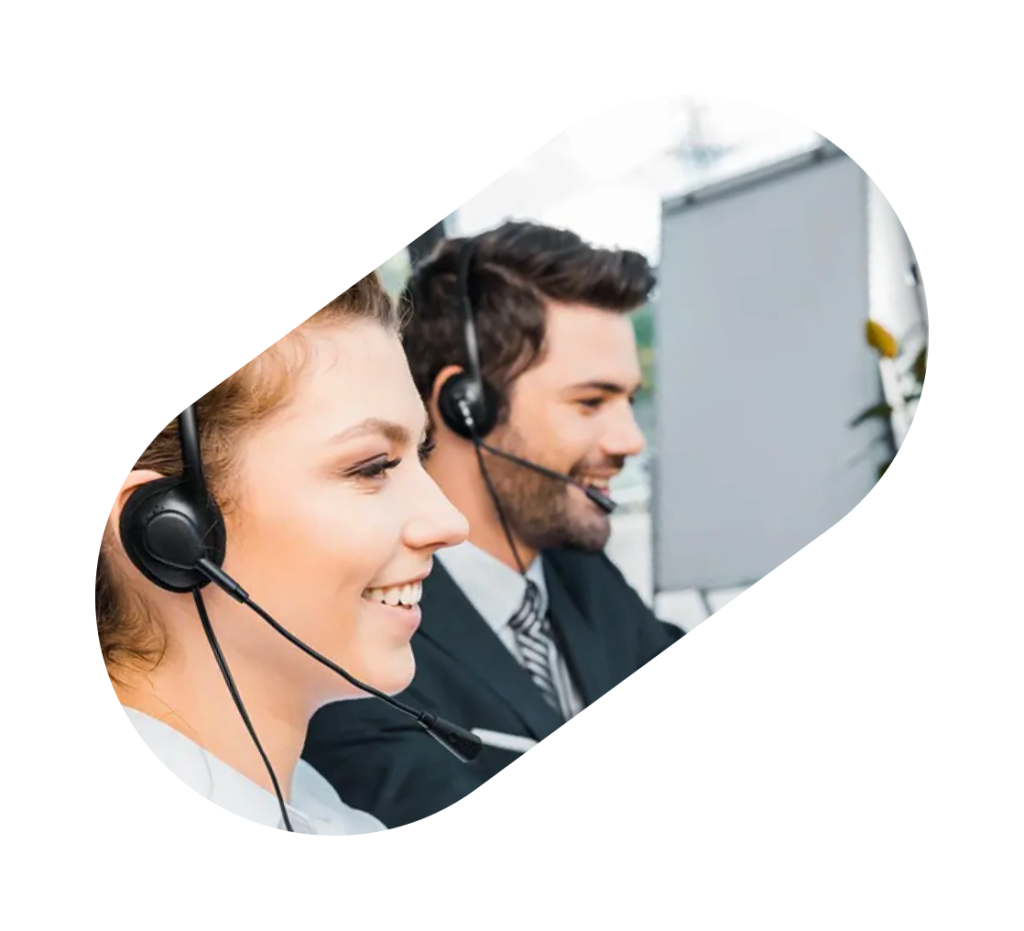
Complete Revenue Cycle Management & Staffing Under One Roof
Serving Physicians, Labs, Nursing Homes, Skilled Nursing, Rehab Centers, Elder Care, Psychologists, Chiropractors, Physical Therapists, Telehealth, Ambulatory Surgical Centers, and Hospice Care.


Our Trusted Client
50%
Collect Cost ↓
30%
Client Revenue Growth
120+
Happy Clients
97%
Collection Rate
Managing a medical practice is demanding. Between treating patients, handling staff, and keeping finances healthy—providers often struggle with billing, authorizations, or staffing shortages. We solve this by bringing everything under one roof:
RCM (Revenue Cycle Management
From eligibility to payment posting, denials, appeals, and patient billing.
Staffing Support
Skilled medical staff, virtual scribes, coders, and back-office support. In collaboration with RIK Healthcare Solutions & Consultant LLP
Practice Growth Partner
Helping you focus on patient care while we handle the rest.
Are these issues holding back the profitability of your practice or facility?
- High claim rejection rates due to eligibility or coding errorsHigh claim rejection rates due to eligibility or coding errors
- Rising billing costs and internal staffing challenges
- Delayed payments from insurance payers
- Constantly changing payer requirements and compliance hurdles
- Lack of performance visibility and outdated reporting
- Missed credentialing renewals and expiring payer contracts
Why Outsource to us?
Specialized Billing Experts:
Years of experience in Labs, Nursing, Skilled Nursing, Rehab Centers, Elder Care, Psychologists, Chiropractors, Physical Therapists, Telehealth, Ambulatory Surgical Centers, Hospice Care, and Labs (Pathology, Genetic, Molecular, Toxicology, and Radiology).
Complete Transparency:
Real-time dashboards, performance metrics, and billing reports accessible 24/7
Scalable Support:
Whether you're a startup lab or a multi-location enterprise
Cost-Efficiency:
Market-beating pricing with flexible models
Compliance First:
HIPAA-compliant, audit-ready documentation with secure access controls
Dedicated Success Manager:
One point of contact for smooth communication

Our Revenue Cycle Management Services
We deliver impactful, cost-efficient revenue cycle solutions see how below.
Patient Scheduling & Requisition
We prevent downstream errors from the first touchpoint by scheduling, confirming, and capturing orders, demographics, and insurance using defined templates and requirements, ensuring accurate appointments, completed intake packets, and reduced no-shows, with confirmations within 24 hours and a ≥15% no-show reduction target.
Eligibility & Benefits Verification (FREE for 1 Months)
We ensure coverage issues are caught before visits through real-time eligibility checks on copays, deductibles, limits, and OON warnings, using insurance details and service codes to provide same-day snapshots for staff and patients, maintaining a ≤1.5% front-end denial rate.
Prior Authorizations / Pre-Certs
We help prevent medical-necessity and “no auth” denials by submitting authorizations with clinicals, tracking expirations/units, and updating the EHR. Using diagnosis, CPT/HCPCS codes, and notes, we secure approvals with dates/units attached to encounters, achieving 95% pre-service auths within 24–72 hrs. Specialty needs include device-specific auths for ASCs and certification alignment for Hospice.
Medical Scribing & Documentation Support
We help reduce provider admin time and improve coding accuracy through live or post-visit scribing, templated notes, and audit cues. By using templates, specialty rules, and provider preferences, we deliver same-day, coding-ready charts that save 1–2 hours daily, with support for specialty needs like psych time-based splits and telehealth POS/modifiers.
Coding (ICD-10/CPT/HCPCS) & Charge Entry
We maximize compliant reimbursement on the first pass by applying accurate codes, modifiers, NCCI edits, and MUE checks. Using finalized notes, op reports, implant logs, and charge tickets, we generate clean, justified charges for claim creation. With a 24–48 hr coding TAT and 97–99% audit accuracy, we ensure speed and precision while addressing specialty needs such as ASC global periods and multiple procedure rules, and chiropractic medical necessity and diagnosis linkage scrutiny.
Claim Scrubbing & Submission (Clearinghouse)
Our purpose is to lift first-pass acceptance and speed up payments by combining automated and manual edits, applying payer rules, submitting EDI, and tracking rejects. We process charges from Stage 5 as inputs and generate submitted claims with tracking IDs as outputs, ensuring a first-pass acceptance rate of at least 98% and submission within 24 hours of coding. For specialties like labs, we handle order-to-claim mapping and reflex testing documentation to maintain accuracy and compliance.
Payment Posting & Reconciliation
Our purpose is to keep the ledger tight and quickly identify underpayments by leveraging ERA/EOB auto-posting with exception handling, applying write-off policies, posting patient responsibilities, and performing bank reconciliations. We work with ERA/EOB feeds and payer contracts as inputs to generate outputs such as daily cash reports and underpayment flags. With strict SLAs and KPIs, we ensure posting within 48 hours of receipt and maintain unapplied cash at less than 1% of monthly receipts. For specialties like hospice, we account for unique requirements such as per-diem versus add-ons and room/board pass-throughs.
AR Follow-Up & Appeals
Our solution is designed to increase patient payments with less friction by providing clear statements, timely SMS and email reminders, easy portal payments, flexible payment plans, and a friendly helpdesk. Using patient contact preferences and the organization’s financial policy as inputs, we drive higher patient collections and reduce front desk complaints. With SLAs such as answering patient calls in under 60 seconds and delivering a typical 10–25% increase in patient collection rates, we ensure measurable improvements. For telehealth, we also provide transparent pre-visit estimates to minimize surprise bills and enhance patient trust.
Denial Management
Our service focuses on fixing root causes and recovering dollars through CARC/RARC coding analysis, rapid corrections, and preventive rule updates. Using denial reason codes and clinical addenda where needed, we deliver accurate resubmissions, a proactive prevention plan, and a monthly denial heatmap. With a strong SLA of maintaining denial rates at or below 4% and ensuring corrected claim turnaround within 3–5 days, we help providers stay compliant and efficient. For specialties such as PT, Chiropractic, and Rehab, we place special emphasis on addressing medical-necessity and documentation frequency denials to minimize revenue loss and strengthen overall claim success.
Patient Billing & Support
We help increase patient payments with less friction through clear statements, SMS/email reminders, portal payments, payment plans, and a supportive helpdesk. Using patient contact preferences and financial policies, we boost collections while reducing complaints, with calls answered under 60 seconds and collection rates typically rising 10–25%. For telehealth, transparent pre-visit estimates further reduce surprise bills and improve trust.
Analytics, Compliance & Continuous Improvement
We help you make informed, audit-ready decisions with weekly dashboards, monthly CFO-ready packs, and quarterly optimization reviews. Covering collections, denials, AR, underpayments, and provider productivity, our HIPAA- and SOC-2–compliant process turns EHR/PM data and payer updates into actionable plans, SOP refinements, and prevention rules—delivered under strict SLAs and KPIs with a 100% audit pass rate.
Specialized BPO for Enterprise Healthcare
Boost operational efficiency and accelerate cash flow with our comprehensive RCM BPO services. We provide end-to-end support including accurate medical coding, thorough audits, insurance eligibility checks, proactive AR follow-up, and effective variance management, ensuring hospitals and healthcare practices minimize revenue leakage, improve compliance, and maximize financial performance.
Simple, Transparent, Flexible
Your Options (pick one or mix & match)
Percentage of Collections (%)
Best for
: End-to-end RCM; aligned incentives.
Includes
: All core RCM stages (1–11) + standard reporting & QA.
Flat Rate per FTE (Dedicated Team)
Best for
Stable volume; want “your” named team (coders, posters, AR).
Includes
Dedicated resources, coverage hours, productivity SLAs.
Per Chart / Per Claim
Best for
Smaller practices, seasonal spikes, testing us in one area (e.g., coding only).
Includes
Clearly defined unit pricing and turnaround SLAs.
Hybrid (Fixed + Variable)
Best for
Clinics wanting predictable base + performance upside.
Includes
Core workflow on fixed retainer; incentive on collections/KPIs.
Project-Based / Cleanup (Hourly or Fixed Bid)
Best for
AR cleanups, backlog coding/posting, short-term coverage.
Includes
Defined scope, sprint plan, and exit report.
Revenue Sharing / Performance Bonuses
Best for
Groups targeting aggressive uplift with shared upside.
Includes
Bonus triggers (e.g., denial rate ≤3%, AR>90 down 40%).
White-Label
Best for
MSOs/Groups—our team works under your brand and systems.
Includes
Branded email/phone, your SOPs, joint QA.
Every healthcare organization has unique needs. Our Quick Chooser guides you to the most effective RCM model for your practice, ensuring efficiency, compliance, and optimized revenue.
Solo/Small Clinic, tight budget
Per Claim or % Collections.
Growing Multi-Specialty
Hybrid (fixed base + upside) or Dedicated FTEs.
Large Facility/ASC/Hospice
Dedicated FTEs + White-Label for brand continuity.
Backlog/AR crisis
Project-Based Cleanup first, then roll into % Collections.
What’s Always Included
We provide secure, automated healthcare solutions with fast claim turnaround, SLA-backed accuracy, weekly reports, and full transition support.
- HIPAA & SOC-2 compliant workflows + signed BAA, encrypted data exchange (FTP, SFTP, VPN).
- Account Manager + escalation matrix (Ops Lead, RCM Lead, Compliance.
- Weekly analytics + Monthly CFO pack and quarterly business reviews.
- Playbook & SOPs tailored to your specialty and payers.
- Disaster recovery & coverage plan (no single-point staffing risk.
- Seamless integration with LIS/EMR (LabDAQ, Orchard, eClinicalWorks, Kareo, etc.
- AI-based claim scrubbing and rule engines
- Automated posting and denial tracking tools
- Secure client portals for documentation and reporting access
Billing & Invoicing
- Frequency: Monthly, in arrears
- Artifacts: Invoice + KPI summary; for %-collections, accompanied by remittance summary.
- Term: Flexible (pilot 90 days; standard 12 months; cancel anytime with notice if pilot).
Q1. What exactly does your RCM service cover?
At Coditi Labs, we provide end-to-end RCM solutions — starting from patient registration, insurance eligibility verification, and medical coding to claim submission, payment posting, denial management, and AR follow-ups. Our goal is to ensure you get maximum reimbursement with minimal delays.
Q2. How do you ensure a high first-pass claim acceptance rate?
Our team uses AI-driven claim scrubbing, automated eligibility checks, and multi-level quality audits to catch errors before submission. As a result, our clients consistently achieve 98–99% first-pass claim acceptance rates, reducing rework and speeding up payments.
Q3. What is your average denial rate and how do you handle denied claims?
We keep denial rates well below the industry average through proactive coding accuracy, pre-authorization checks, and payer rule monitoring. When denials occur, our denial management specialists analyze root causes, resubmit corrected claims within 24–48 hours, and implement prevention measures.
Q4. How do you keep up with changing payer rules and compliance requirements?
Our RCM team undergoes regular training on ICD-10, CPT, and HCPCS updates. We closely monitor payer bulletins, state regulations, and CMS guidelines to ensure compliance. We are fully HIPAA-compliant with robust internal audits and security protocols in place.
Q5. What kind of reports and analytics will I receive?
We provide executive-ready, real-time dashboards and monthly performance reports covering KPIs like collections, days in AR, denial trends, and net collection rates. Our analytics help you make data-driven decisions to improve cash flow and operational efficiency.
Q6. Can you integrate with my existing EHR/PM system?
Yes. Coditi Labs has experience working with all major EHR and practice management platforms including Epic, Cerner, Athenahealth, eClinicalWorks, NextGen, and custom-built systems. We ensure smooth data migration, interoperability, and minimal disruption during onboarding.
Q7.What’s your pricing model?
We offer flexible pricing — percentage of collections, flat monthly fee, or a hybrid model — depending on your needs. Our pricing is transparent with no hidden charges, ensuring you get a measurable ROI from our services.
Q8. How do you ensure data security and patient privacy?
We follow HIPAA, HITRUST, and SOC 2 standards. All data is encrypted in transit and at rest, with strict access controls and continuous monitoring. We conduct regular security audits to safeguard PHI and maintain complete confidentiality.
Q9. How quickly can we expect to see improvements in cash flow?
Many clients see noticeable improvements within 60–90 days of onboarding. Our process optimization, denial reduction strategies, and faster payment cycles ensure steady cash flow growth from the first quarter.
Q10. Do you offer specialty-specific RCM expertise?
Absolutely. Our team has specialized billing expertise across multiple specialties including cardiology, orthopedics, behavioral health, dentistry, urgent care, and more. We adapt workflows and coding guidelines to fit your specialty’s unique requirements.